Introduction to Public Health
The Development of the discipline of Public Health
What is Health?
The question ‘What is health?’ is not an easy one to answer. United Nations officials had to ponder it when, in 1948, they founded the World Health Organization (WHO). They came up with the following: ‘Health is a complete state of physical, mental and social well-being and not merely the absence of disease or infirmity, a definition that has been widely cited ever since.
Many people do think of health, primarily, as the absence of disease. Diagnosing and treating disease is the central focus of most health systems and at the core of traditional medical school curricula. Tackling disease is seen as the primary route to improving health – and there has been considerable success in doing so.
In many parts of the world, the government action to improve health has been far less convincing, and healthcare systems continue to focus on the absence of disease, rather than taking the more holistic view that the World Health Organization’s definition suggests. For example, in the Conservative government’s financial statement in the autumn of 2015, despite the need to find funds to pay down a deficit, a major increase was made in funding for the National Health Service (NHS), largely to address pressures in hospital services, while public health budgets were cut.
In the late 1960s, the leading British public health thinker Thomas McKeown of Birmingham said, ‘The disposal of society’s investment in health is based on strange premises. It is assumed that we are ill and made well, whereas it is nearer to the truth that we are well and made ill. Fifty years on, it is difficult to dispute the continuing validity of this telling observation when the policies of many health ministries are viewed in the cold light of day.
Health in a Changing World
In the mid-1980s, the World Health Organization published the Ottawa Charter for Health Promotion. It followed the first major global conference to address the concept of health promotion, which is now a mainstream component of public health. The Ottawa Charter developed the idea of health as a fundamental human right, and identified a few prerequisites for it, including Peace, Food, Shelter, Education, Income, Sustainable resources, A sustainable ecosystem, Social justice, and equity.
The Ottawa Charter saw it as more helpful to define the social and physical resources required for health and focus on improving those, rather than defining health at the individual level. The original World Health Organization definition of health is more than half a century old. Some see its statement that health is a state of complete well-being as unhelpful. Very few people are completely well in every way, and on a pedantic view of the definition, most people are therefore unhealthy. As people age, many begin to accumulate chronic, non-communicable diseases. Arguably, a more helpful definition would not write them all off as failing to attain a complete state of physical, mental, and social well-being.
The World Health Organization’s original definition also says nothing about what physical, social, or mental well-being means, simply stating that health requires each of these to be ‘complete’. Some maintain that the definition has led to an ideal of perfect health and that this utopian notion has fed an increasing medicalization of society’s problems.
Historical markers in the development of Public Health
The history of public health goes back to almost if the history of civilization. Possible traditions during civilization may be, taboos against waste disposal within communal areas or near drinking water sources; rites associated with the burial of the dead; and communal assistance during birth.
In the Ancient Societies (before 500 BC) the history is that of archaeological findings from the Indus valley (North India) around 2000 BC with the evidence of bathrooms and drains in homes and sewer below street level. There was evidence of drainage systems in the middle kingdom of ancient Egypt in the time 2700 -2000 BC. There were written records concerning public health, codes of Hamurabi of Babylon, 3900 years ago.
The Book of Leviticus (1500 BC) had guidelines for personal cleanliness, sanitation of campsites, disinfection of wells, isolation of lepers, disposal of refuses, and hygiene of maternity.
In the Classical Cultures (500 BC - 500 AD) public health was practiced as Olympics for physical fitness, community sanitation and water wells in the era golden age of ancient Greek; and aqueducts to transport water, sewer system, regulation on street cleaning and infirmaries for slaves by Romans.
In the middle ages (500 - 1500 AD), health problems were considered as having spiritual causes and solutions. They were supernatural powers for pagans and punishments for sins for Christians. Leprosy, plague (Black Death) during the 14th century and syphilis were some of the deadliest epidemics resulted from failure to consider the physical and biological causes.
The era of renaissance and exploration (1500 – 1700 AD) was the rebirth of thinking about the nature of the world and humankind. There was a growing belief that diseases were caused by the environment, not by spirits, and critical thinking about disease causation e.g., "malaria" - bad air.
In the eighteen centuries, there were problems of industrialization, urban slums leading to unsanitary conditions and unsafe workplaces. Edward Jenner (1796) demonstrated vaccination against smallpox.
Twentieth-century has been the period of health resources development (1900-1960), social engineering (1960 - 1973), health promotion (Primary Health Care), and market period (1985 and beyond).
The challenge in the twenty-first century is reducing the burden of excess morbidity and mortality among the poor; counter reacting the threats of economic crisis, unhealthy environment, and lifestyle; developing a more effective health system and investing in expanding knowledge base.
The scope and concerns of Public Health
There have been many definitions and elaborations of public health. The definition offered by the Acheson Report has been widely accepted:
Public health is the science and art of preventing disease, prolonging life, and promoting health through the organized efforts of society.
[This definition underscores the broad scope of public health and the fact that public health is the result of all of society’s efforts viewed as a whole, rather than that of single individuals].
In 2003, Roger Detels defined the goal of public health as:
The biological, physical, and mental well-being of all members of society regardless of gender, wealth, ethnicity, sexual orientation, country, or political views.
[This definition or goal emphasizes equity and the range of public health interests as encompassing not just the physical and biological, but also the mental well-being of society].
The United Nation’s Millennium Development Goals, the slogan of which is ‘Health for All’ (the Acheson report), and Detels’ goals depict public health as being concerned with more than the mere elimination of disease and placing public health issues as a fundamental component of development.
To achieve the World Health Organization (WHO) the goal of health for all, it is essential to bring to bear many diverse disciplines to the attainment of optimal health, including the physical, biological, and social sciences. The field of public health has adapted and applied these disciplines for the elimination and control of disease, and the promotion of health.
What is Public Health?
Public health is defined as the science and art of preventing diseases, prolonging life, promoting health and efficiencies through organized community effort. It is concerned with the health of the whole population and the prevention of disease from which it suffers. It is also one of the efforts organized by society to protect, promote, and restore people's health. It is the combination of sciences, skills, and beliefs that are directed to the maintenance and improvement of the health of all people through collective social actions. People who work in the diverse field of public health actively contribute to building and sustaining healthy communities. In your community today, public health practitioners may be found:
Public Health – An introduction
Public health is about protecting and improving the health of whole populations and communities. Its motivation is to improve the health of individual people. But unlike clinical medicine, which focuses on people one at a time, public health takes a broader focus to understand and engage with the many factors (societal, behavioral, and environmental) that promote or undermine health.
Public health emphasizes the promotion of health and the prevention of disease and disability; the collection and use of epidemiological data; population surveillance and other forms of empirical quantitative assessment; a recognition of the multidimensional nature of the determinants of health; and developing effective solutions to population health problems.
Any list of activities and projects carried out by a department of public health would be lengthy and diverse and not necessarily consistent with a similar list produced by another department in the same country or in a different country. That is why perusing such lists or reading and talking about public health programs often gives a better and a clearer understanding of what public health is about than memorizing a formal definition.
Public health practice can involve tackling huge issues that affect the whole world, such as the health effects of climate change, as well as quite circumscribed and small-scale interventions, such as introducing new hygiene procedures at a local children’s animal petting farm after an outbreak of serious illness caused by the bacterium Escherichia coli.
While most of the core concepts of public health has remained the same for many decades, there have been three big shifts of emphasis from the late twentieth century into the twenty-first century.
First, the paradigm of public health is no longer national; it is global. Second, public health is no longer only the domain of professionals. Health system managers and political leaders have had to become engaged to address the challenges of new threats to health and the growing burden of potentially preventable, non-communicable diseases. Third, pursuing effective solutions for problems that are mainly multi-factorial in causation and influenced by broader environmental, social, and economic conditions require interdisciplinary practice and multi-agency, multi-sector cooperative working.
Functions of Public Health
Public health is concerned with the process of mobilizing local, state/provincial, national, and international resources to assure the conditions in which all people can be healthy. To successfully implement this process and to make health for all achievable, public health must perform the functions listed here:
Prevent disease and its progression, and injuries.
Promote healthy lifestyles and good health habits.
Identify, measure, monitor, and anticipate community health needs (e.g., surveillance).
Investigate and diagnose health problems, including microbial and chemical hazards.
Formulate, promote, and enforce essential health policies.
Organize and ensure high quality, cost-effective public health, and healthcare services.
Reduce health disparities and ensure access to healthcare for all.
Promote and protect a healthy environment.
Disseminate health information and mobilize communities to take appropriate action.
Plan and prepare for natural and man-made disasters.
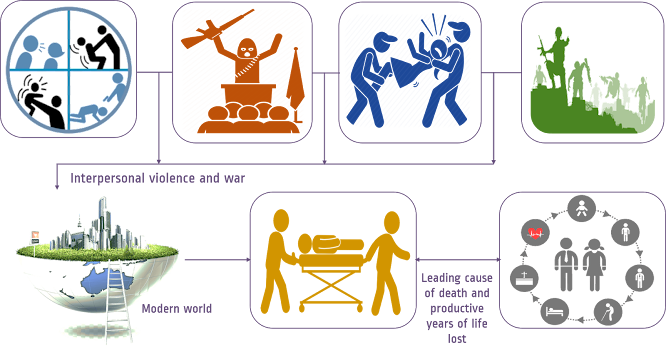
Reduce the impact of interpersonal violence and aggressive war.
Conduct research and evaluate health-promoting/disease-preventing strategies.
Develop new methodologies for research and evaluation.
Train and ensure a competent public health workforce.
Over the last century, the quality of research has been enhanced by the development of new methodologies, particularly in the fields of epidemiology, bio-statistics, and laboratory sciences. Rapid advances in computational hardware and techniques have increased our ability to analyze massive amounts of data and to use multiple strategies to aid in the interpretation of data. Despite this, it will be a major challenge to keep pace with the explosive growth in the volume and complexity of data being generated, driven by a range of factors from the pervasive use of the Internet, social media, and mobile phones, to the masses of data from molecular biology and sequencing studies. Glean valuable insights pertinent to public health from these huge datasets will require new approaches, strategies, and methodologies. It is essential that public health continues to use leading-edge technologies to develop more sophisticated research strategies to address public health issues.
A major problem in public health has been translating research advances into effective health practice and policy in a timely manner. A new area of research, implementation science, has been proposed to delineate barriers to and factors that facilitate rapid translation of scientific advances into improvements in health practice and development of more effective policies promoting health. The quality of public health is dependent on the competence and vision of the public health workforce. Thus, it is an essential function of public health to ensure the continuing availability of a well-trained, competent workforce at all levels, including leaders with the vision essential to ensure the continued well-being of society and the implementation of innovative, effective public health measures.
Finally, a thread that runs through all these functions is the necessity for much greater international collaboration in data sharing, policy formulation and implementation, and the management of specific public health issues. With globalization, the rapid flow of information, people, goods, and services across national boundaries mean that many public health concerns and issues are interconnected in complex ways. Effective solutions will therefore often depend on joint action between different countries. In addition, now more than ever, there are many opportunities for major public health attainments to be made through cooperative action at the global level, as has been demonstrated in the past by milestones such as the eradication of smallpox. The media can play an important role in educating the public and in facilitating public health interventions.
Public health identifies, measures, and monitors health needs and trends at the community, national, and global levels through surveillance of disease and risk factors (e.g., smoking) trends. Analysis of these trends and the existence of functioning health information system provides the essential information for predicting or anticipating future community health needs.
To ensure the health of the population, it is necessary to formulate, promote, and enforce sound health policies to prevent and control disease, and to reduce the prevalence of factors impairing the health of the community. These include policies requiring reporting of highly transmissible diseases and health threats to the community and control of environmental threats through the regulation of environmental hazards (e.g., water and air quality standards and smoking). It is important to recognize that influencing politics and policies is an essential function of public health at the local, national, and global levels.
There are limited resources that can be devoted to public health and the assurance of high-quality health services. Thus, an essential function of public health is to effectively plan, manage, coordinate, and administer cost-effective health services, and to ensure their availability to all segments of society. In every society, there are health inequalities that limit the ability of some members to achieve their maximum ability to function. Although these disparities primarily affect the poor, minority, rural, and remote populations and the vulnerable, they also impact society, particularly regarding infectious and/or transmissible diseases. Thus, there is not only an ethical imperative to reduce health disparities, but also a pragmatic rationale.
Contemporary Health Issues
Technological advances and increasing commerce have done much to improve quality of life, but these advances have often come at a high cost to the environment. In many cities of both the developed and developing world, the poor quality of air—contaminated by industry and commerce—has affected the respiratory health of the population, and has threatened to change the climate, with disastrous consequences locally and globally. We have only one world. If we do not take care of it, we will ultimately have difficulty living in it. Through the education of the public, formulation of sound regulations, and influencing policy, public health can contribute much to the protection and monitoring of the environment to ensure that it is conducive for the population to live healthily.
We cannot predict, and rarely can we prevent, the occurrence of natural and man-made disasters, but we can prepare for them to ensure that the resulting damage is minimized. Thus, disaster preparedness is an essential component of public health, whether the disaster is an epidemic such as influenza or the occurrence of typhoons and other natural disaster.







Super sir👍👍👍👍👍👍👍
ReplyDeleteSuper
ReplyDeleteSuper
ReplyDeleteSuper
ReplyDeleteGreat initiative. Looking forward to see more
ReplyDeleteNice
ReplyDeleteVery well scripted
ReplyDeleteNice
ReplyDeleteGreat initiative
ReplyDeleteNice
ReplyDeleteLooking forward to read more from you
ReplyDeleteGood
ReplyDeleteThis is my first time visit to your blog and I am very interested in the articles that you serve. Provide enough knowledge for me. Thank you for sharing useful and don't forget, keep sharing useful info: medical care equipment and supplies
ReplyDeleteHello, I have gone through your article on improving eating habits and I found it really very informative. You know, you write the same thing which I was searching for. Thanks a lot for your efforts. Keep Posting. If you want to enroll in an Online Medical Laboratory Technician Course , visit Virohan for that.
ReplyDelete